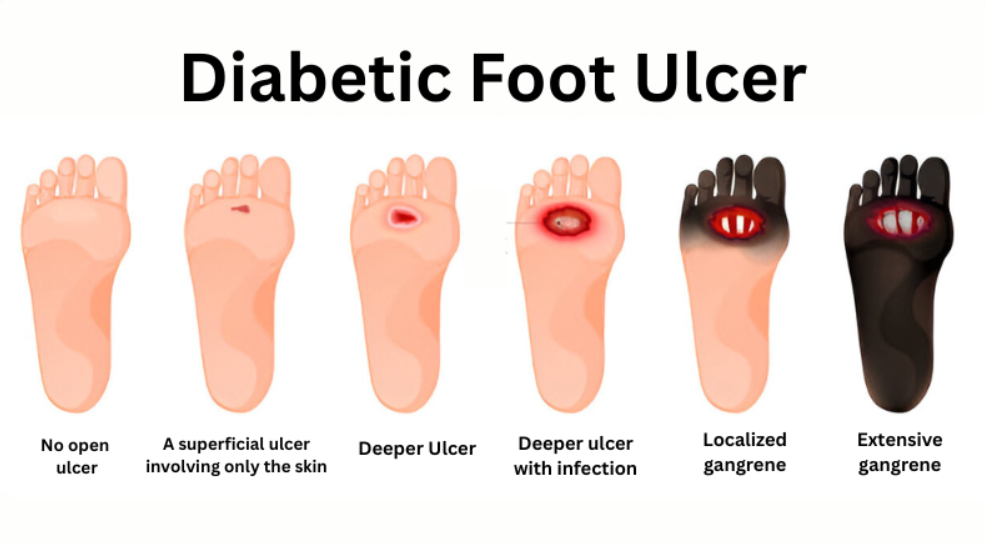
Foot ulcers in people with diabetes are a serious issue. They can start small and become severe if not noticed early. As a general surgeon in Gurgaon, I often see cases where ulcers are ignored until complications arise. Understanding the early-stage diabetic foot ulcer and its worsening stages helps in treating wisely and prevents the need for diabetic foot treatment.
Let me walk you through the five stages of a diabetic foot ulcer. This way, you can identify problems early and seek help before things get harder to manage.
Stage 1: Skin Redness or Callus
This is where it often starts. You might feel a hard spot or see a red patch on the foot, especially over bony areas like heels or toes. It could be a callus or slight swelling. Pain may be mild or absent. Many normalize it as shoe friction. But this is a warning sign.
At this point, good foot hygiene, cutting toenails properly, and avoiding tight footwear can prevent ulcers from forming. I advise scheduling a foot exam as soon as you notice persistent redness or callus.
Stage 2: Superficial Ulcer
If Stage 1 is ignored, the callus may break, forming a sore that stays open. This ulcer is shallow. You might see a pink or red base. Surrounding skin may look inflamed. Discharge might begin—usually clear or yellowish.
Regular dressing changes, gentle cleaning, and offloading pressure (not standing too much) help this stage heal. However, if the ulcer doesn’t improve within a few weeks, it’s time to consult. Early care prevents progression.
Stage 3: Deep Ulcer to Tendons
Here, the wound deepens. You may see tendons, ligaments, or even a bit of bone. Pain may be more noticeable. Discharge increases and may smell unpleasant. The risk of infection grows significantly.
At this stage, more than dressings are needed. We perform debridement—removing dead tissue in the clinic. You may need antibiotics. We also start looking at circulation. In my practice, I do an ultrasound or ankle-brachial index to check blood flow. Healing becomes a team effort—wound care nurse, podiatrist, and I working together.
Stage 4: Bone Infection (Osteomyelitis)
When bacteria reach the bone, it’s called osteomyelitis. The skin may turn red, swollen, and warm. The area feels sore. Fever or chills can happen. These are signs of a deep infection. We act fast.
To confirm bone involvement, I usually order an X-ray or MRI. If infection is present, surgery is often needed. We remove infected tissue, and sometimes part of the bone. This is what we mean by diabetic foot treatment—the goal is to stop the spread and save the foot.
After surgery, I prescribe antibiotics based on your reports. Medicines support recovery, but surgery is key when the infection goes that deep.
Stage 5: Severe Infection & Gangrene
This is the most serious stage. Tissue may turn black, gangrene. The area becomes cold, numb, and foul-smelling. Pain may be severe or absent because of nerve damage.
At this stage, immediate care is critical. Surgery often involves removing dead tissue. In worst cases, partial or full amputation is needed. I’ve had to do this when infection risks the patient’s life. After surgery, rehabilitation and footwear change are essential to prevent further issues.
Early Stages Matter Most
Not every stage progresses to the worst. But neglect at Stage 1 or 2 can push you up the scale quickly.
I strongly encourage regular foot checks if you have diabetes:
- Inspect daily with a mirror—under toes and heels
- Use gentle soap and dry well
- Apply moisturizer—but not between the toes
- Seek help for wounds that don’t heal in 7–10 days
A Surgeon's Approach to Healing
I approach these ulcers with both medical care and foot-saving intent. My steps include:
- Thorough exam—check blood flow, sensation, and infection.
- Early debridement and cleaning.
- Imagine when bone involvement is suspected.
- Antibiotic dosing based on lab results.
- Wound dressing and offloading pressure.
- Surgical removal of infected tissue (if needed).
- Education on footwear adjustment.
- Close follow-up to prevent recurrence.
As a best general surgeon in gurgaon, I take a no-delay approach. No one should suffer or risk losing a limb. Every stage has options for healing, comfort, and mobility.
Final Thoughts
A diabetic foot early stages ulcer might seem minor. But left alone, it's often not minor for long. Spotting changes early saves foot function and even your life. I’m ready to help with effective care, careful surgery if needed, and full support throughout recovery.